10 Oct How Flat Feet Can Lead to Other Health Issues and How to Treat Them
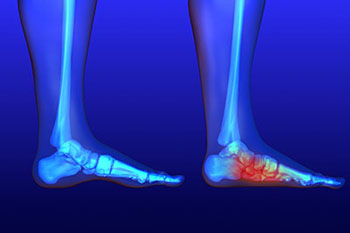
Flat feet occur when the arches of the feet flatten, allowing the entire sole to touch the floor when standing. This condition can be present from childhood or may develop during adulthood. The structural change in the foot’s mechanics influences the ankles, knees, hips, and lower back. Altered alignment, balance, and the distribution of weight throughout the body may result from these changes.
What Causes Flat Feet?
The development of flat feet can be attributed to several factors. For many individuals, low arches are a congenital trait, meaning they are present from birth due to genetics. In adults, a common cause is posterior tibial tendon dysfunction. The posterior tibial tendon is a primary support structure for the foot’s arch. When this tendon becomes weakened or inflamed from overuse or injury, it no longer adequately support the arch, leading to its gradual collapse. Repetitive load from high-impact activities or prolonged standing can place stress on the foot and contribute to this condition.
What Issues Do They Cause?
Individuals with flat feet may experience a range of symptoms, though some people have no discomfort at all. A common complaint is discomfort or an aching sensation in the arch or heel area. Some people report experiencing pain in their hips or lower back, which can be linked to the changes in their gait and posture.
A visible sign of flat feet is the inward rolling of the ankles, a motion known as overpronation. This altered gait mechanism contributes to strain in the lower leg. The change in foot alignment may also affect how the knee tracks, potentially leading to knee discomfort.
How Are They Treated?
The management of flat feet is typically focused on alleviating symptoms and improving foot function. Activity modifications, such as reducing the duration of high-impact exercises or periods of prolonged standing, can help manage symptoms. Professionally fitted insoles or custom orthotics can be inserted into shoes to provide additional support to the arch and help correct alignment issues.
Targeted strengthening and mobility exercises from physical therapy can be beneficial. Stretching routines for the calves and the Achilles tendon may also be suggested to improve flexibility. Balance and gait training can help improve body mechanics during movement.
In some cases, a brace may be used to support the foot and ankle. Imaging studies may be ordered to evaluate the structure of the foot and the condition of the tendons. If symptoms persist and limit daily function, a surgeon may discuss surgical options.
Consult a Foot Specialist
If you experience persistent foot pain, notice changes in the shape of your feet, or find that symptoms are interfering with your daily activities, seeking a professional evaluation is a logical next step. A foot specialist, such as a podiatrist, can perform a thorough examination to determine the underlying cause of your symptoms. This assessment may involve observing your gait, examining the structure of your feet, and reviewing your medical history. Based on this evaluation, the specialist can provide a tailored management plan to address your specific needs and help you maintain an active lifestyle.

No Comments